Medical Credentialing Services for Providers & Clinics in Minnesota


Why Credentialing Matters for Minnesota Healthcare Providers
- Claim denials
- Credentialing delays
- Delayed reimbursements
- Loss of network access with major commercial and government payers
Why Credentialing Matters for Minnesota Healthcare Providers
We offer end-to-end provider credentialing in Minnesota for a wide range of specialties and practice types.
From initial credentialing to lifecycle maintenance, we handle every aspect of your enrollment and stay on top of changing compliance requirements.
Our services include:
NPI Type 1 and Type 2 Registrations
Our team assists with National Provider Identifier (NPI) registration and payer enrollment, whether you're an individual provider (Type 1) or a group/facility (Type 2).
Primary Source Verification
From initial credentialing to recredentialing, we manage every step, starting with primary source verification of licenses, education, malpractice, and work history.
CAQH ProView Profile Setup and Maintenance
Set up and manage your CAQH ProView profile for accurate, attested, and up-to-date information. We track re-attestation deadlines and keep your documents compliant with Minnesota commercial payers.
Payer Credentialing Applications Submission
We submit and track payer applications with commercial and government plans, ensuring all data meets NCQA and payer-specific standards.
Recredentialing
We also handle ongoing recredentialing requirements of the insurance providers across Minnesota guidelines, so you remain active and billing-eligible.
MN Medicaid Credentialing (MA) and Medicare Enrollment
Expert support for enrolling providers with Minnesota Medicaid (MA) and Medicare through CMS. Our team navigates the complex application and verification processes to help you gain participation quickly.
Group and Facility Enrollment with Commercial Payers, Medicare, and Medicaid
We handle group and facility credentialing across commercial payers, Medicare, and Minnesota Medicaid.
Credentialing Process We Follow
1. Application Initiation
2. Verification & Validation
3. Payer Submission
4. Approval & Follow-up
Local Minnesota Payers & Networks We
Work With



your applications move forward without unnecessary delays.
Cities & Regions We Serve Across Minnesota






Who Needs Credentialing Services?
- MDs, DOs, NPs, PAs
- Therapists, LCSWs, mental health professionals
- Solo practices, multi-provider clinics, urgent care centers
Why Choose MinnesotaBillingServices.com?
- Minnesota-based credentialing specialists who understand local payer nuances
- Payer liaisons who handle follow-ups and escalate issues
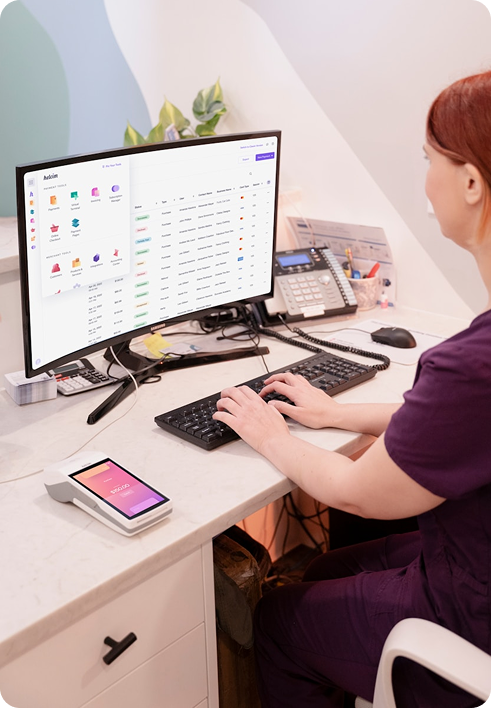
- Credentialing automation tools that streamline every step
- Compliance-driven, error-free credentialing with full-cycle support
Frequently Asked Questions (FAQs)
Ready to Get Credentialed Fast?
Provider onboarding help
A free credentialing audit to assess your current gaps
