Wound Care Billing Services – Specialized Support for Minnesota Clinics

At Minnesota Billing, we specialize in wound care billing services for clinics, home health agencies, and wound care centers across Minnesota. Our dedicated team of experts is trained in CPT codes for chronic wounds, NPWT billing, wound debridement billing, and other specialized billing requirements to ensure accurate reimbursement and fewer denials. We are your trusted wound care billing experts, adept at navigating Medicare Local Coverage Determinations (LCDs), payer-specific rules, and skin substitute applications. Let us handle your revenue cycle so you can focus on providing top-quality care to your patients.
Why Choose Minnesota Billing for Wound Care Billing?
Expertise in Wound Care Coding and Payer Nuances
Navigating the world of wound care billing requires an in-depth understanding of wound care-specific coding, such as the use of CPT codes for chronic wounds, including debridement (97597/97598) and negative pressure wound therapy.
Familiarity with Minnesota Medicaid & Medicare MAC Rules
Our team is well-versed in the intricacies of Minnesota Medicaid and Medicare rules. We ensure that your billing process complies with local regulations and Medicare Advantage Plans, minimizing denials and accelerating reimbursement..
Specialized Team Trained in Wound Debridement, Skin Substitutes, and NPWT
Whether it’s wound debridement billing, skin substitute applications (CPT 15271, 15278), or NPWT billing, our specialized team ensures accuracy in coding and compliance with the latest payer policies.
Common CPT & HCPCS Codes We Master
The wound care billing process requires familiarity with a wide range of CPT and HCPCS Level II codes. Here are some of the most commonly used codes that our team expertly handles:
Debridement
- CPT 97597/97598: Debridement of chronic wounds.
- CPT 11042–11047: Debridement for different types of wounds, including minor and major procedures.
NPWT (Negative Pressure Wound Therapy)
- CPT 97605/97606: Codes for the application of NPWT, essential for chronic wound care.
- HCPCS 97607–97608: Codes for disposable NPWT, often used in outpatient and home health settings.
Skin Substitute Application
Documentation & Billing Best Practices
Track Wound Size, Type, and Drainage Evolution
Use NPWT and Skin Graft Documentation Standards
Manage NCCI Edit Conflicts and Use Modifiers Effectively

Our Service Workflow for Wound Care Clinics
Eligibility & Coverage Checks
Accurate Coding by Certified Coders
Claim Submission, Denial Follow-Up, and AR Tracking
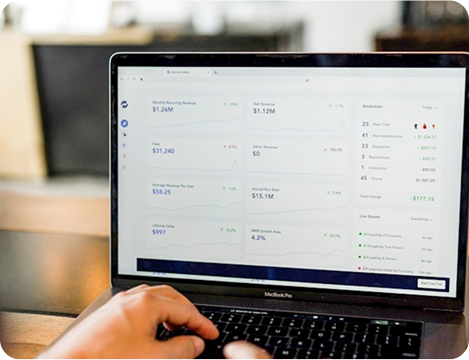
Monthly KPI Dashboards